Causes, Symptoms and Treatment Options
Medically reviewed on May 21, 2018 What Is It? 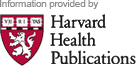 Asthma is a chronic (long-term) lung condition. Air passages narrow and become inflamed. This leads to breathing difficulties and wheezing. Asthma ranges from mild to severe. Some people have only occasional, mild symptoms. Others have nearly constant symptoms with severe, life-threatening flare-ups. During an asthma attack, the airways become more inflamed than usual. They narrow as the muscles surrounding them constrict. Mucus produced by the inflammation fills the narrowed passageways. As a result, the flow of air is partially or completely blocked. Asthma affects the lung's larger and smaller airways.
Asthma is a chronic (long-term) lung condition. Air passages narrow and become inflamed. This leads to breathing difficulties and wheezing. Asthma ranges from mild to severe. Some people have only occasional, mild symptoms. Others have nearly constant symptoms with severe, life-threatening flare-ups. During an asthma attack, the airways become more inflamed than usual. They narrow as the muscles surrounding them constrict. Mucus produced by the inflammation fills the narrowed passageways. As a result, the flow of air is partially or completely blocked. Asthma affects the lung's larger and smaller airways.  A variety of environmental asthma "triggers" have been identified. Many of them are allergens. Allergens cause the immune system to overreact in some people. Common allergens include: Animal dander and saliva Pollens Molds Dust mites Cockroaches Some medications Certain foods Also high on the list of asthma triggers are: Viral infections, such as colds and influenza Exercise Breathing cold, dry air Environmental pollutants, such as: Cigarette smoke Wood smoke Paint fumes Chemicals Strong odors Emotional stress For some people with severe asthma, no specific triggers can be identified. Asthma can develop early, often before age 5. But its symptoms can begin at any age. The condition has a genetic (inherited) component. It often affects people with a family history of allergies. Symptoms Symptoms of asthma include: For some people with asthma, a chronic cough is the main symptom. Symptoms of a severe asthma attack can include: Extreme shortness of breath Chest tightness A rapid pulse Sweating Flared nostrils and pursed lips A need to sit upright A bluish discoloration of the lips and fingernails Between asthma attacks or flare-ups, people with mild or moderate asthma may not have any symptoms. In some people, symptoms flare up only during or after exercise. People with asthma tend to have more severe symptoms when they have an upper respiratory infection such as a cold or the flu. Diagnosis Your doctor will ask about: Any symptoms you have How severe they are When and where they occur How frequently they occur What triggers and relieves them These details will help your doctor find ways to help prevent your. asthma attacks. Your doctor also will want to know about: Your personal history of allergies and respiratory illnesses Your family history of asthma, allergies and respiratory illnesses Your doctor will listen to your back with a stethoscope to detect wheezing. During an attack, your doctor can assess the severity of your flare-up. He will listen for the amount of airflow in your lungs. He will also observe how you are using your chest muscles to breathe. Blue lips or skin are a sign that you are not getting enough oxygen. Your doctor may check your peak air flow with a peak-flow meter. It provides a quick and easy measurement of air flow from the lungs. It measures the speed of air expelled when you blow forcibly through it. Peak-flow meters often are given to asthma patients for use at home. They can use them to monitor their asthma. These devices help to detect the earliest signs of an asthma flare-up. Another test, called pulse oximetry, measures oxygen levels in your blood. It is done by placing a small plastic clip on the tip of your finger. Your doctor may order another test called spirometry. This is a more thorough test of lung function. It is used to confirm an asthma diagnosis and help assess severity. During spirometry, you exhale into a device that analyzes the amount and volume of airflow. One part of the test may be repeated after you are given a bronchodilator. This medication relaxes the muscles surrounding the airways. If airflow improves with a bronchodilator, it indicates that you have asthma. Sometimes a challenge test is done when spirometry appears normal. For this test, you inhale a medication to see if it causes your airway muscles to tighten up. People with asthma are more sensitive to this medication: their airway muscles are more likely to tighten up. Your doctor may want to do a blood test or allergy skin testing. These tests are used to determine specific substances ("allergens") that can trigger an allergy. During a severe asthma flare-up, an arterial blood gas (ABG) test may be done to provide a more accurate measure of your oxygen level. The test also provides information about the seriousness of the attack. Your doctor also may want you to have a chest X-ray. Expected Duration Asthma in adults often is a lifelong condition. With treatment, symptoms can be controlled. They can be infrequent or very mild. In about half of asthmatic children, the asthma goes away on its own. Or it becomes less severe over time. However, it often reappears later in life. Asthma episodes can go away on their own or with the help of asthma medications. Attacks vary in frequency and severity. It is often dependent on what triggers the attack. Prevention Some asthma episodes can be prevented by avoiding or minimizing exposure to triggers. These include environmental triggers such as: If exercise triggers your asthma: Breathe warm, humidified air before and during exercise Use inhalers before exercise Eliminating allergens at home often can go a long way to control asthma symptoms. If dust mites are a trigger: Encase mattresses in airtight enclosures Clean your home frequently Wash bedding frequently in very hot water Remove carpets and heavy draperies from sleeping areas Some people may need to avoid animals entirely. Others may benefit from taking preventive medicine before an anticipated exposure to animals. Pet owners should keep pets out of bedrooms and bathe them regularly. Those who are affected by pollens should: Prevention also means learning to anticipate future attacks. Monitor your symptoms and peak-flow readings to help identify a coming attack before symptoms develop. This allows you to adjust your medications to prevent an attack. Early signs or symptoms of an asthma flare-up include: Coughing more often Increased mucus or phlegm Becoming short of breath quickly with exertion or exercise Developing a sinus headache or fever Having symptoms that resemble a cold: Runny or congested nose Sneezing Watery eyes Treatment Treatment focuses on: If you have chronic asthma, work with your doctor to write an asthma-management plan. The plan specifies: How to avoid asthma triggers When and how regular medications should be taken How to handle acute attacks How a peak-flow meter should be used Several types of medication are available to treat asthma. Some treat acute attacks (the "quick relievers"). Others prevent attacks from happening (the "controllers"). It is important to take preventive asthma medications as prescribed. You should take them even when you are not having symptoms. Bronchodilators. Bronchodilators relax the muscles around the airways to improve airflow. They are commonly inhaled. One class of bronchodilators is called beta agonists. It includes albuterol, metaproterenol, and pirbuterol. Beta agonists can be prescribed alone as quick relievers, for mild, occasional symptoms. They also are used as "rescue" medications to stop an attack. They can be inhaled in an inhaler or taken with a nebulizer. A nebulizer is a device that mixes medications with a mist for inhalation. Other long-acting bronchodilators are used as "controllers" to reduce the number of asthma attacks. These include salmeterol (Serevent) and formoterol (Foradil, Perforomist). They are not useful for an asthma attack because they take too long to begin working. People using a daily long-acting bronchodilator must also use a daily corticosteroid inhaler. People with asthma that only use a long-acting bronchodilator may have an increased risk of death.
A variety of environmental asthma "triggers" have been identified. Many of them are allergens. Allergens cause the immune system to overreact in some people. Common allergens include: Animal dander and saliva Pollens Molds Dust mites Cockroaches Some medications Certain foods Also high on the list of asthma triggers are: Viral infections, such as colds and influenza Exercise Breathing cold, dry air Environmental pollutants, such as: Cigarette smoke Wood smoke Paint fumes Chemicals Strong odors Emotional stress For some people with severe asthma, no specific triggers can be identified. Asthma can develop early, often before age 5. But its symptoms can begin at any age. The condition has a genetic (inherited) component. It often affects people with a family history of allergies. Symptoms Symptoms of asthma include: For some people with asthma, a chronic cough is the main symptom. Symptoms of a severe asthma attack can include: Extreme shortness of breath Chest tightness A rapid pulse Sweating Flared nostrils and pursed lips A need to sit upright A bluish discoloration of the lips and fingernails Between asthma attacks or flare-ups, people with mild or moderate asthma may not have any symptoms. In some people, symptoms flare up only during or after exercise. People with asthma tend to have more severe symptoms when they have an upper respiratory infection such as a cold or the flu. Diagnosis Your doctor will ask about: Any symptoms you have How severe they are When and where they occur How frequently they occur What triggers and relieves them These details will help your doctor find ways to help prevent your. asthma attacks. Your doctor also will want to know about: Your personal history of allergies and respiratory illnesses Your family history of asthma, allergies and respiratory illnesses Your doctor will listen to your back with a stethoscope to detect wheezing. During an attack, your doctor can assess the severity of your flare-up. He will listen for the amount of airflow in your lungs. He will also observe how you are using your chest muscles to breathe. Blue lips or skin are a sign that you are not getting enough oxygen. Your doctor may check your peak air flow with a peak-flow meter. It provides a quick and easy measurement of air flow from the lungs. It measures the speed of air expelled when you blow forcibly through it. Peak-flow meters often are given to asthma patients for use at home. They can use them to monitor their asthma. These devices help to detect the earliest signs of an asthma flare-up. Another test, called pulse oximetry, measures oxygen levels in your blood. It is done by placing a small plastic clip on the tip of your finger. Your doctor may order another test called spirometry. This is a more thorough test of lung function. It is used to confirm an asthma diagnosis and help assess severity. During spirometry, you exhale into a device that analyzes the amount and volume of airflow. One part of the test may be repeated after you are given a bronchodilator. This medication relaxes the muscles surrounding the airways. If airflow improves with a bronchodilator, it indicates that you have asthma. Sometimes a challenge test is done when spirometry appears normal. For this test, you inhale a medication to see if it causes your airway muscles to tighten up. People with asthma are more sensitive to this medication: their airway muscles are more likely to tighten up. Your doctor may want to do a blood test or allergy skin testing. These tests are used to determine specific substances ("allergens") that can trigger an allergy. During a severe asthma flare-up, an arterial blood gas (ABG) test may be done to provide a more accurate measure of your oxygen level. The test also provides information about the seriousness of the attack. Your doctor also may want you to have a chest X-ray. Expected Duration Asthma in adults often is a lifelong condition. With treatment, symptoms can be controlled. They can be infrequent or very mild. In about half of asthmatic children, the asthma goes away on its own. Or it becomes less severe over time. However, it often reappears later in life. Asthma episodes can go away on their own or with the help of asthma medications. Attacks vary in frequency and severity. It is often dependent on what triggers the attack. Prevention Some asthma episodes can be prevented by avoiding or minimizing exposure to triggers. These include environmental triggers such as: If exercise triggers your asthma: Breathe warm, humidified air before and during exercise Use inhalers before exercise Eliminating allergens at home often can go a long way to control asthma symptoms. If dust mites are a trigger: Encase mattresses in airtight enclosures Clean your home frequently Wash bedding frequently in very hot water Remove carpets and heavy draperies from sleeping areas Some people may need to avoid animals entirely. Others may benefit from taking preventive medicine before an anticipated exposure to animals. Pet owners should keep pets out of bedrooms and bathe them regularly. Those who are affected by pollens should: Prevention also means learning to anticipate future attacks. Monitor your symptoms and peak-flow readings to help identify a coming attack before symptoms develop. This allows you to adjust your medications to prevent an attack. Early signs or symptoms of an asthma flare-up include: Coughing more often Increased mucus or phlegm Becoming short of breath quickly with exertion or exercise Developing a sinus headache or fever Having symptoms that resemble a cold: Runny or congested nose Sneezing Watery eyes Treatment Treatment focuses on: If you have chronic asthma, work with your doctor to write an asthma-management plan. The plan specifies: How to avoid asthma triggers When and how regular medications should be taken How to handle acute attacks How a peak-flow meter should be used Several types of medication are available to treat asthma. Some treat acute attacks (the "quick relievers"). Others prevent attacks from happening (the "controllers"). It is important to take preventive asthma medications as prescribed. You should take them even when you are not having symptoms. Bronchodilators. Bronchodilators relax the muscles around the airways to improve airflow. They are commonly inhaled. One class of bronchodilators is called beta agonists. It includes albuterol, metaproterenol, and pirbuterol. Beta agonists can be prescribed alone as quick relievers, for mild, occasional symptoms. They also are used as "rescue" medications to stop an attack. They can be inhaled in an inhaler or taken with a nebulizer. A nebulizer is a device that mixes medications with a mist for inhalation. Other long-acting bronchodilators are used as "controllers" to reduce the number of asthma attacks. These include salmeterol (Serevent) and formoterol (Foradil, Perforomist). They are not useful for an asthma attack because they take too long to begin working. People using a daily long-acting bronchodilator must also use a daily corticosteroid inhaler. People with asthma that only use a long-acting bronchodilator may have an increased risk of death.  Anti-inflammatory medications. These are controllers. They are usually taken regularly, regardless of whether a person is having asthma symptoms. They work by reducing inflammation. This decreases mucous production and reduces constriction of airway muscles. Anyone with asthma symptoms that occur more than a couple times per week should consider taking an anti-inflammatory medication. The first choice is usually an inhaled corticosteroid. Corticosteroids also can be taken as pills when inhaled corticosteroids are not completely successful. People requiring emergency care or hospitalization often receive corticosteroids intravenously. Other inhaled anti-inflammatories are also available. Leukotriene modifiers are taken by mouth. These drugs block chemicals that cause inflammation and airway narrowing in many people with asthma. Another anti-inflammatory medicine is omalizumab (Xolair), which blocks inflammation by attacking IgE antibodies. IgE antibodies are major players in allergic reactions. This drug helps control symptoms in people with severe allergic asthma that is unresponsive to other therapies and requires frequent oral corticosteroids. Long acting bronchodilator/corticosteroid combination inhalers. There are several products that combine these two agents in a single product. Examples include Advair, Symbicort and Dulera. Immunotherapy. Some people with asthma also benefit from immunotherapy. In immunotherapy, the person is injected with increasing amounts of allergens. The aim is to desensitize the person's immune system. Immunotherapy appears to be most effective for mild to moderate asthma symptoms caused by sensitivity to indoor allergens. Severe asthma attacks must be treated in a hospital. There, oxygen can be administered, and drugs may be given intravenously or with a nebulizer. In life-threatening cases, the patient may need a breathing tube placed in the large airway and artificial ventilation. When To Call A Professional Call your doctor whenever you or your child has persistent: Wheezing Chest tightness Difficulty breathing Cough Some children with asthma may not complain specifically of shortness of breath. However, they may flare their nostrils or use their chest and neck muscles when breathing. These are signs that they are having trouble. If you already have been diagnosed with asthma, call your doctor if your symptoms: For example, call your doctor if you must use your rescue bronchodilator more than four times a day. Also call if your peak-flow-meter readings are in the yellow or red zones. If you have an asthma attack and your symptoms persist despite your usual medications, seek emergency help immediately. Prognosis Although asthma cannot be cured, it almost always can be controlled successfully. Most people with asthma lead relatively normal lives. Learn more about AsthmaAssociated drugsMicromedex® Care NotesSymptom checkerMayo Clinic ReferenceExternal resources American Academy of Allergy, Asthma & Immunology (AAAAI)555 East Wells St. Suite 1100Milwaukee, WI 53202-3823 Phone: (414) 272-6071Toll-Free: (800) 822-2762 http://www.aaaai.org/ American Lung Association61 Broadway, 6th FloorNew York, NY 10006br />Phone: (212) 315-8700Toll-Free: (800) 548-8252 http://www.lungusa.org/ National Institute of Allergy and Infectious Diseases (NIAID) Office of Communications & Public Liaison5601 Fishers Lane, MSC 9806Bethesda, MD 20892-9806For deliveries, use Rockville, MD 20852Phone: (301) 496-5717http://www.niaid.nih.gov/ Further informationAlways consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.Medical Disclaimer
Anti-inflammatory medications. These are controllers. They are usually taken regularly, regardless of whether a person is having asthma symptoms. They work by reducing inflammation. This decreases mucous production and reduces constriction of airway muscles. Anyone with asthma symptoms that occur more than a couple times per week should consider taking an anti-inflammatory medication. The first choice is usually an inhaled corticosteroid. Corticosteroids also can be taken as pills when inhaled corticosteroids are not completely successful. People requiring emergency care or hospitalization often receive corticosteroids intravenously. Other inhaled anti-inflammatories are also available. Leukotriene modifiers are taken by mouth. These drugs block chemicals that cause inflammation and airway narrowing in many people with asthma. Another anti-inflammatory medicine is omalizumab (Xolair), which blocks inflammation by attacking IgE antibodies. IgE antibodies are major players in allergic reactions. This drug helps control symptoms in people with severe allergic asthma that is unresponsive to other therapies and requires frequent oral corticosteroids. Long acting bronchodilator/corticosteroid combination inhalers. There are several products that combine these two agents in a single product. Examples include Advair, Symbicort and Dulera. Immunotherapy. Some people with asthma also benefit from immunotherapy. In immunotherapy, the person is injected with increasing amounts of allergens. The aim is to desensitize the person's immune system. Immunotherapy appears to be most effective for mild to moderate asthma symptoms caused by sensitivity to indoor allergens. Severe asthma attacks must be treated in a hospital. There, oxygen can be administered, and drugs may be given intravenously or with a nebulizer. In life-threatening cases, the patient may need a breathing tube placed in the large airway and artificial ventilation. When To Call A Professional Call your doctor whenever you or your child has persistent: Wheezing Chest tightness Difficulty breathing Cough Some children with asthma may not complain specifically of shortness of breath. However, they may flare their nostrils or use their chest and neck muscles when breathing. These are signs that they are having trouble. If you already have been diagnosed with asthma, call your doctor if your symptoms: For example, call your doctor if you must use your rescue bronchodilator more than four times a day. Also call if your peak-flow-meter readings are in the yellow or red zones. If you have an asthma attack and your symptoms persist despite your usual medications, seek emergency help immediately. Prognosis Although asthma cannot be cured, it almost always can be controlled successfully. Most people with asthma lead relatively normal lives. Learn more about AsthmaAssociated drugsMicromedex® Care NotesSymptom checkerMayo Clinic ReferenceExternal resources American Academy of Allergy, Asthma & Immunology (AAAAI)555 East Wells St. Suite 1100Milwaukee, WI 53202-3823 Phone: (414) 272-6071Toll-Free: (800) 822-2762 http://www.aaaai.org/ American Lung Association61 Broadway, 6th FloorNew York, NY 10006br />Phone: (212) 315-8700Toll-Free: (800) 548-8252 http://www.lungusa.org/ National Institute of Allergy and Infectious Diseases (NIAID) Office of Communications & Public Liaison5601 Fishers Lane, MSC 9806Bethesda, MD 20892-9806For deliveries, use Rockville, MD 20852Phone: (301) 496-5717http://www.niaid.nih.gov/ Further informationAlways consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.Medical Disclaimer



/https%3A%2F%2Fsyndwire-videos-new.s3.amazonaws.com%2Fnbypq1549889432.jpg)
/https%3A%2F%2Fassets.over-blog.com%2Ft%2Fcedistic%2Fcamera.png)